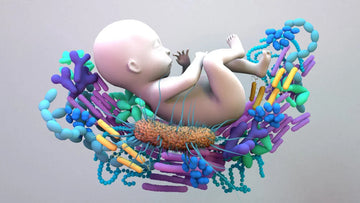
Vaginal seeding is a procedure in which a newborn delivered by cesarean section is exposed to the mother’s vaginal microbes. This is done by swabbing the mother's vaginal fluids onto the newborn's skin, mouth, and eyes shortly after birth to help introduce beneficial bacteria. The practice aims to mimic some microbial exposure that babies naturally receive during vaginal delivery, as these microbes may play a role in developing a healthy immune system and gut microbiome. However, vaginal microbiota transfer is controversial and not widely recommended due to potential risks, including the transmission of vaginal infections. Understanding the procedure’s benefits and risks is essential for making informed decisions.
What is Vaginal Seeding?
Vaginal seeding, also known as vaginal microbiota transfer(VMT), is a practice intended to transfer beneficial bacteria from a mother's birth canal to her newborn, particularly for babies delivered by cesarean section(c- section). During a vaginal birth, a baby is naturally exposed to the mother's vaginal microbiota, which plays a crucial role in establishing the baby's initial microbiome, a community of bacteria essential for immune system development and gut health.

Babies born via C-section miss this initial exposure and may be at a higher risk for certain immune-related conditions, such as asthma, allergies, and obesity. Vaginal microbiota transfer involves swabbing the mother's vaginal fluids and applying them to the newborn's skin, mouth, and nose shortly after birth to mimic the microbiome exposure of vaginal hygiene. While some studies suggest this could help balance the baby's microbiome, the practice is still considered experimental, and medical guidelines urge caution due to the potential risk of infection.
The Procedure of Vaginal Seeding
This procedure aims to transfer the mother's microbiota to the baby, potentially helping the infant develop a balanced and healthy microbiome similar to that acquired during a vaginal birth. Here’s an outline of how vaginal microbiota transfer is generally performed:
Preparation
In preparation for vaginal seeding, a sterile gauze or cotton swab is used to collect the mother’s vaginal discharge or fluids. This step usually happens just before the C-section or immediately afterward to ensure the bacteria are fresh and viable. Sterility is crucial, as it reduces the risk of introducing any contaminants that could harm the baby.
Application to The Baby
Once the gauze or swab has collected a sample, it is gently wiped across the newborn’s body, focusing on areas where bacteria colonization is most effective, such as the mouth, face, and body. This is thought to help replicate the natural exposure that a baby would experience during vaginal delivery, where the baby passes through the birth canal and comes into contact with the mother’s microbiota.
By applying these bacteria early, vaginal microbiota transfer aims to promote the development of a healthy microbiome in the newborn, which can influence immune system function and digestion and potentially reduce the risk of certain health issues, including allergies, asthma, and autoimmune diseases.
Timing and Hygiene
Timing is essential in vaginal seeding because exposure to beneficial bacteria is most effective immediately after birth. This early introduction helps to "seed" the baby’s microbiome during the critical window when the immune system is still developing. Introducing the mother's microbiota at this point can promote early colonization of the baby’s gut and skin, which may help to outcompete harmful bacteria. Strict hygiene protocols are followed to prevent the transmission of any harmful bacteria or contaminants.
Medical Supervision
Vaginal seeding should always be done under the supervision of healthcare professionals. Before the procedure, doctors conduct thorough screenings to ensure that the mother is free of infections or other health conditions that could pose a risk to the baby. Medical supervision also helps address any concerns or questions that parents may have regarding the procedure's safety and potential benefits. Currently, there is limited but growing research on the benefits and risks associated with vaginal microbiota transfer, and healthcare providers can help parents make an informed choice based on the latest evidence.
Why is Vaginal Seeding Done?
Vaginal seeding is a practice aimed at transferring beneficial bacteria from the mother to a newborn, especially in cases where the baby is delivered via cesarean section. Babies born vaginally are naturally exposed to their mother’s vaginal microbiome, which plays a critical role in seeding their immune system with beneficial bacteria, potentially reducing their risk for various health issues such as allergies, asthma, and immune-related disorders.
During a C-section, however, babies miss out on this exposure, as they are born directly from the uterus without contact with the vaginal canal. To mimic this process, some mothers choose to swab the baby with gauze or cloth that has been exposed to the vaginal area immediately after birth. Though some early studies have shown promising results, vaginal microbiota transfer remains a controversial practice. Medical professionals debate its safety and effectiveness, as there is a potential risk of transferring harmful bacteria alongside beneficial ones.
Benefits of Vaginal Seeding
Vaginal seeding, also known as micro birthing, involves swabbing a newborn delivered via cesarean section with the mother’s vaginal fluids. This is done to expose the infant to the beneficial bacteria present in the vaginal canal, similar to what a baby born through a vaginal birth would naturally encounter.
Microbiome Development
When babies are born vaginally, they pass through the birth canal, where they encounter and pick up a complex mix of beneficial bacteria from their mother’s vaginal microbiome. Babies born via cesarean section miss this initial exposure to maternal vaginal bacteria. Instead, they tend to acquire skin and environmental bacteria, which results in a different bacterial profile from babies born vaginally. By using vaginal microbiota transfer, healthcare providers attempt to mimic the natural exposure to maternal bacteria.
Enhanced Immune System
The microbiome directly influences the development of the immune system. Early exposure to maternal bacteria, especially from the placenta, plays a role in “training” the newborn immune system to distinguish between harmful and harmless bacteria between This helps condition the immune system to respond appropriately to the pathogen and reduces the chance of overreaction to non-threatening stimuli (characteristic of many autoimmune allergies around).
Reduced Risk of Allergies and Asthma
Babies without exposure to various bacteria at birth may be more prone to these conditions because their immune systems may react more to foreign substances. Studies have shown that children with higher microbiome diversity tend to have lower asthma rates, eczema, and allergies. Early bacterial exposure, particularly to beneficial bacteria from the mother, may help regulate immune responses and prevent an overreaction to allergens.
Supportive Digestive Health
Babies born through vaginal delivery are thought to have an advantage in developing a gut microbiome that supports these functions, thanks to early bacterial exposure. By using vaginal microbiota transfer, healthcare providers aim to introduce similar beneficial bacteria to C-section babies, potentially aiding in the formation of a healthy gut microbiota. A well-established gut microbiota also contributes to a strong immune response and a balanced metabolism, both critical to overall health.
Risks Involved in Vaginal Seeding
While vaginal transfer of microorganisms can be beneficial, it carries some risks, especially because of the possible transfer of infection from mother to baby. Suppose the mother carries infections such as group B streptococcus (GBS), herpes simplex virus, HIV, and chlamydia. When that happens, the baby can be introduced to this pathogen, causing serious complications, especially because the immune system of the newborn is immature. If procedures are not followed, appropriate sterilization procedures and handling are followed accurately, even with the risk of swabbing or gauze.
Conclusion
vaginal seeding offers a novel way to mimic the natural bacterial transfer that occurs during labor and can contribute to the growth of healthy gut microbiota in children whose newborns are delivered by C-section. While it can offer benefits, such as reduced risk of acne and improved immune function, the procedure is not without risks with possible maternal infection transmission of the vaginal mucosa and should therefore be administered under medical supervision, taking careful consideration of the health status of the mother. As research continues to evolve, parents and healthcare professionals should be informed and cautious in adopting this upcoming intervention, and also pregnancy care is much more important for vaginal delivery.
FAQ’s
Why Is Vaginal Seeding Performed?
Vaginal microbiota transfer is ideally performed immediately after delivery, within the first few hours of the baby’s life, to maximize the introduction of beneficial bacteria.
What Are The Benefits Of Vaginal Microbiota Transfer?
Potential benefits include promoting a diverse and healthy gut microbiome, enhancing immune system development, and reducing the risk of conditions like allergies, asthma, and obesity later in life.
Is Vaginal Microbiota Transfer Safe For All Mothers And Babies?
Vaginal microbiota transfer is not recommended for mothers with known infections or health conditions that could harm the baby. It should only be performed under medical supervision, following thorough screening.
Can Vaginal Seeding Replace Breast Feeding?
No, vaginal microbiota transfer is not a substitute for breastfeeding. Breastfeeding remains crucial for providing essential nutrients and antibodies that support the infant's immune system and overall health.
What Are The Risk Associated With Vaginal Seeding?
The primary risks involve the transmission of maternal infections, such as group B streptococcus, herpes, and other pathogens, which can pose serious health risks to the newborn, especially if the mother is not screened for infections beforehand.